Improve Employee Benefits Without Increasing Healthcare Costs
A preventive care and wellness program that helps employers enhance benefits and improve payroll efficiency — without changing existing health insurance.
Lower payroll tax exposure
No out-of-pocket cost to employees
Upgrade benefits without raising premiums
CLICK BELOW TO WATCH FIRST!
Used by employers to find hidden payroll savings
Why Employers Are Re-Evaluating Benefits
Employers are under increasing pressure:
Health insurance costs continue to rise
Employees expect more support beyond traditional coverage
Raising wages isn’t always sustainable
Many benefits don’t improve retention or utilization

The Preventative Care Management Program (PCMP) offers a comprehensive range of benefits aimed at improving employee health, promoting financial wellness, and generating savings for employers.
Ignite Primary Benefits
WELLNESS & PREVENTATIVE BENEFITS
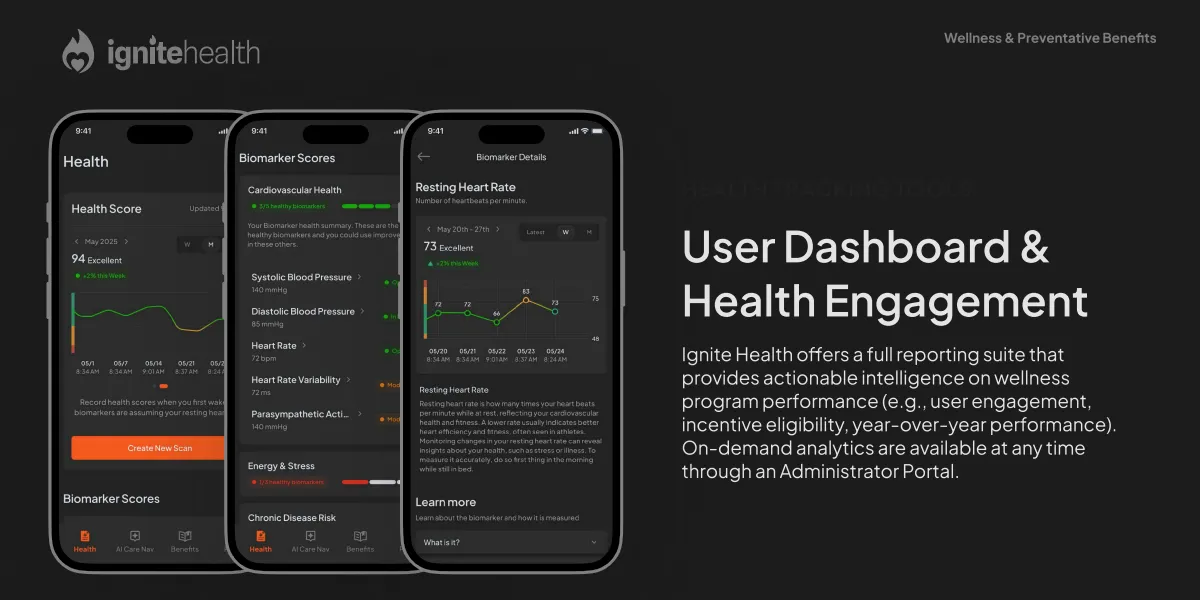
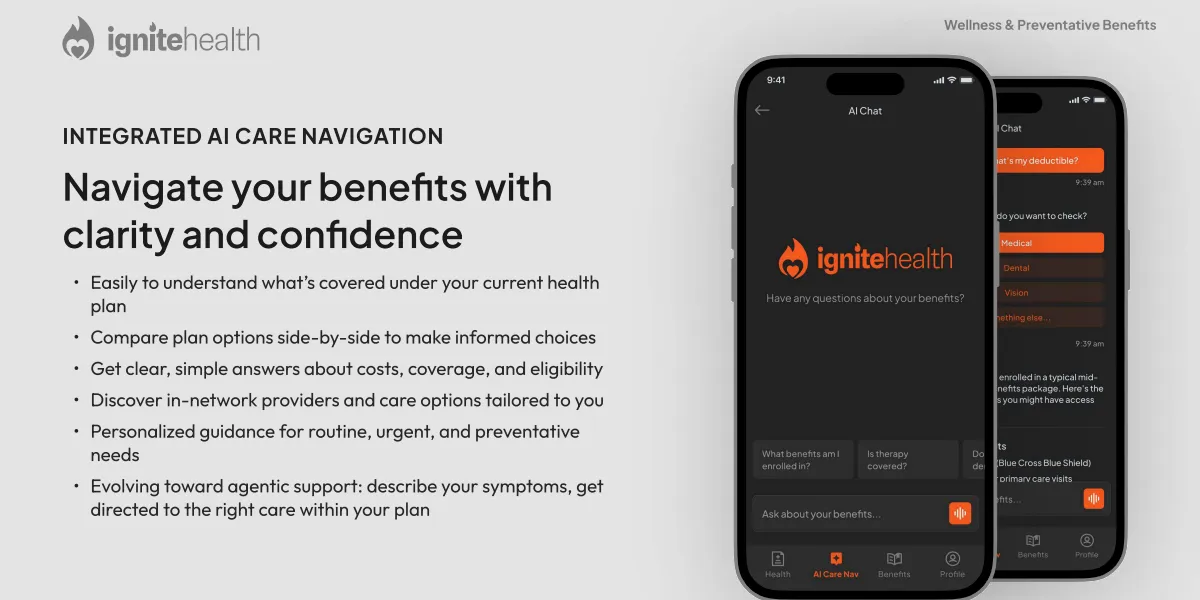
Ignite Health Platform
Access behavior tools, risk resolution guides, health tracking, videos, and resources — all in one hub.
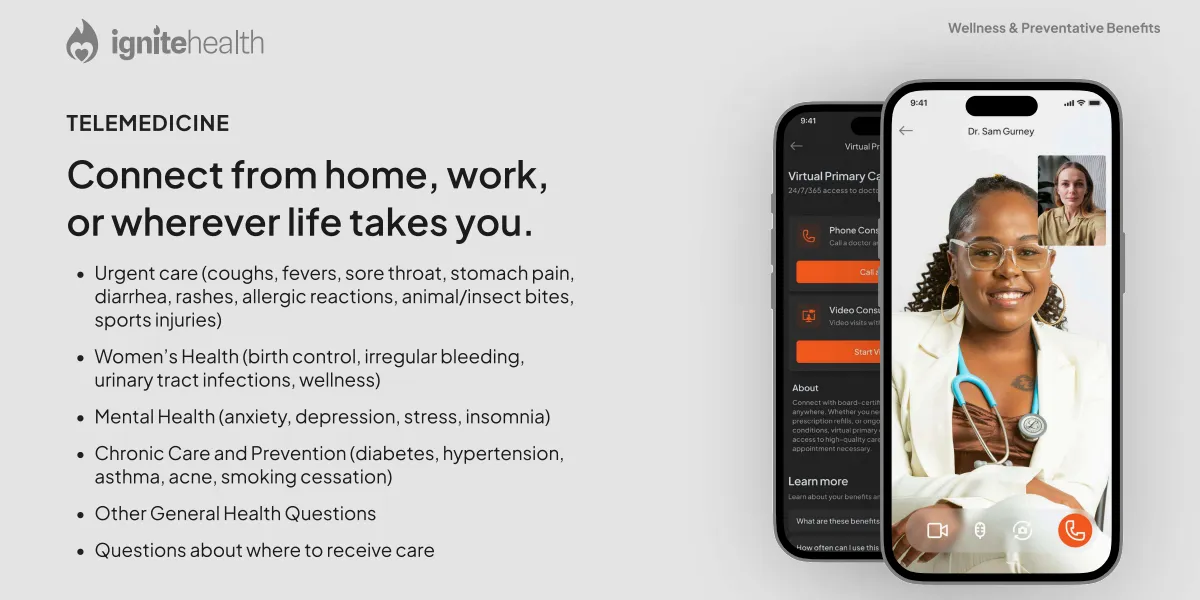
Telemedicine
Unlimited virtual visits with licensed practitioners, available 24/7/365 for the whole family — with no copay.
Wholestic™ Coaching
Unlimited nurse-led coaching to help you and your family understand, manage, and improve overall health.
Mental Health & Wellness Support
Screenings and counseling for depression, substance use, and behavioral health — promoting long-term mental well-being.
Women’s Health Benefits
Comprehensive women’s care including mammograms, Pap tests, prenatal and reproductive health, and cancer prevention.
Comprehensive Health Screenings
Routine checks for cancer, diabetes, hypertension, cholesterol, and obesity — to detect, manage, and prevent health issues early
Preventive Care & Immunizations
Free vaccines (flu, HPV, shingles, and more) plus screenings for blood pressure, cholesterol, and diabetes.
Employee Assistance Program
Confidential support for work-life balance, stress, and resilience — at no cost to employees.
Prescription Drug Coverage
Free prescriptions for employees and families, covering 1,000+ medications at 70,000+ pharmacies nationwide.
Please Note – These benefits are only a portion of the 19 total Mayo Clinic benefits included in the Preventative Care Management Program.
All associated benefits are included at no out-of-pocket expense to the employee, and do not include any individual co-pay.
A Smarter Way to Deliver Preventive Care
The Preventive Care Management Program (PCMP) is a structured wellness and preventive care program designed to support employee health while improving payroll efficiency.
The program is built to:
Improve the employee benefit experience
Reduce unnecessary payroll tax exposure
Operate alongside existing health insurance, not replace it
All eligibility, compliance, payroll coordination, and employee enrollment are handled by the program administrator.
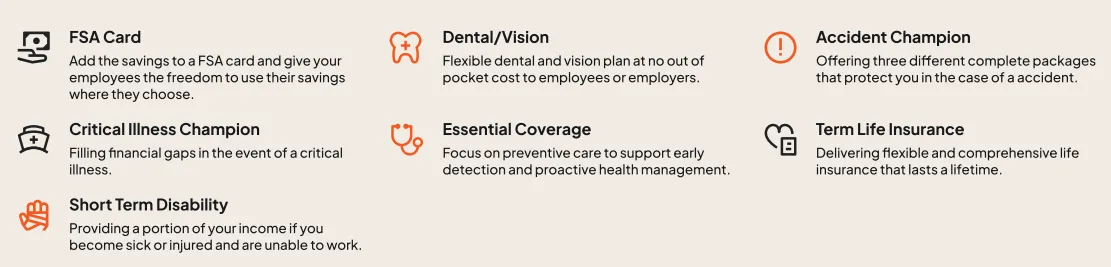
Supplemental & Essential Benefits
Supplemental & Essential Benefits
We support individuals and their families during challenging times by offering policies that provide essential coverage and cash benefits for covered accidents and illnesses. These benefits are designed to help ease financial burdens and provide the support you need when it matters most.
How The Program Works
1. Review
Review Your Workforce & Payroll
Share a recent payroll report and a few details about your team so we can assess fit and estimate potential savings under a compliant Section 125 structure.
You’ll see how preventive care and wellness can be funded by reallocating existing payroll tax dollars, not adding new benefit spend.
2. Design
Design Your Preventive Care Program
If there is a fit, the program administrator builds a customized preventive care and wellness plan that runs alongside your current health insurance.
All eligibility, compliance, and payroll coordination are handled for you, so your HR and finance teams are not burdened with extra administration.
3. Implement
Implement, Enroll, and Realize Savings
Employees are enrolled into the program and gain access to expanded preventive, mental health, and telemedicine benefits with no reduction in net take-home pay.
You begin seeing improved benefits and potential payroll tax efficiencies, supported by ongoing administration and reporting from the third-party specialist.
Ready to get started?
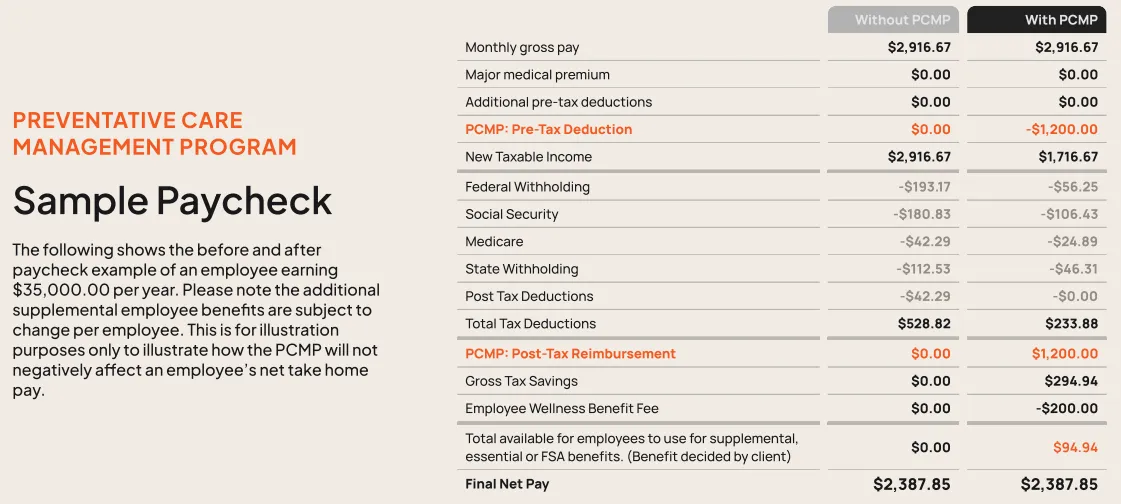
How the Program Is Funded
PCMP is funded through existing payroll tax savings, not increased healthcare spend.
By structuring eligible preventive care benefits through a compliant framework:
Employers may reduce payroll tax liability
Employees receive expanded benefits
No increase in premiums or wages is required
Payroll impact and examples are reviewed in advance, so employers can clearly see how the program works before making any changes.
Who Typically Benefits Most
This program is often a good fit for employers with:
10–250 W-2 employees
Payroll-heavy or hourly workforces
Rising benefit or payroll pressure
An interest in retention and cost control
Common industries include trades, manufacturing, hospitality, healthcare practices, professional services, and multi-location businesses.
What the Review Process Looks Like
Book a short benefits review call
Eligibility and workforce fit are reviewed
Payroll examples are shared before implementation
You decide whether to move forward
No pressure. No obligation.
See If This Makes Sense for Your Business
The benefits review call is a working session — not a sales pitch.
You’ll get clarity on fit, funding, and next steps.
TESTIMONIALS
What others are saying
Frequently Asked Questions
Does this replace our current health insurance?
No.
The Preventive Care Management Program is designed to run alongside your existing health insurance, not replace it.
The program includes Minimum Essential Coverage (MEC) as part of the overall structure, which supports access to preventive care and ACA alignment. However, it is not major medical insurance and does not replace your current health plan or broker relationships.
Will this increase our healthcare costs or premiums?
No.
The program is designed to improve benefits without increasing healthcare premiums or total benefit spend. It is funded through existing payroll tax savings, not new employer contributions.
Payroll examples are reviewed in advance so you can clearly see the impact before making any decisions.
Does this reduce employee take-home pay?
No.
The program is structured so employees receive access to expanded preventive and wellness benefits without a reduction in net take-home pay.
This is reviewed and confirmed during the onboarding process before anything is implemented.
Is this complicated to administer or manage internally?
No.
The program is administered by a third-party specialist who handles:
Eligibility review
Compliance
Payroll coordination
Employee enrollment
Employers are not responsible for day-to-day administration or employee benefit questions related to the program.
What is the next step if we want to explore this?
The next step is a short benefits review call.
During that call, the administrator:
Reviews eligibility and workforce fit
Explains how the program works alongside your current benefits
Walks through payroll examples
There is no obligation to move forward after the review.
Still have questions?
The benefits review call is the fastest way to determine whether this makes sense for your business.
This program is designed to operate within applicable IRS and ACA regulations. Participation depends on eligibility and proper administration. This information is not tax or legal advice.